Contents of Article
- Summary
- Why is hydration important for athletes?
- What is hydration testing?
- Why is hydration testing important?
- How is hydration measured?
- Are there any issues with hydration testing?
- Is future research needed with hydration testing?
- Conclusion
- References
- About the Author
Summary
The practice of hydration testing has been implemented for the past couple of decades, with new and more advanced technology capable of detecting smaller changes in an athlete’s hydration status becoming available in more recent years. Hydration status can influence a range of physiological functions in the human body relating to both performance and health, therefore, regular testing is advised.
Many forms of hydration testing exist, most of which are discussed in this article. For any practitioner, it is essential to fully understand the validity or reliability of the testing method, and how this can be compromised in different situations.

Why is hydration important for athletes?
Staying hydrated each day is crucial for many reasons: to regulate body temperature, keep joints lubricated, prevent infections, deliver nutrients to cells, and keep organs functioning properly. Being properly hydrated also improves sleep quality, cognition, and mood. In addition to this, dehydration also impairs sports performance. Ensuring athletes are properly hydrated is therefore very important.
Exercise or physical activity takes place in many different environmental conditions, for example, in climates which vary greatly in terms of temperature and humidity. This, in conjunction with a range of other factors, such as fitness level and metabolic rate, can cause an increase in core body temperature and effectively increase perspiration (i.e. sweating) (1). In humans, the primary method of heat loss is sweating (2), and this can be substantial during vigorous exercise, especially in warm and humid environments.
Sweat not only contains water but also electrolytes which are important for the optimal function of the human body (3). Loss of these important molecules can not only have a detrimental effect on performance, but also on health (4), and as such, it is useful to implement protocols capable of detecting these changes in hydration status. Hydration testing can take many forms depending on the available resources and how much time the practitioner is willing to dedicate to it.
This article will summarise the three main methods often used to assess hydration status in athletes, as well as common issues associated with these methods. It is important to note there is not one particular method which suits everybody in every scenario, instead, the practitioner must carefully consider which method is right for them and their athlete(s).
What is hydration testing?
Hydration testing is a protocol used to determine an athlete’s body fluid balance. An athlete with a normal body fluid balance is said to be euhydrated (5). This euhydrated status is not a specific point, but rather a state of normal body water. Disturbances to an athlete’s body fluid balance can cause severe performance and health defects (3, 4) hence why hydration testing can be a useful component of athletic programmes. When the athlete is in their euhydrated state, they are more likely to be able to perform at their full capacity than if they are dehydrated (6).
Many hydration testing methods have been developed and implemented, the most common of which include:
- Body Weight Changes
- Bioelectrical Impedance Analysis
- Urine Specific Gravity
- Urinary indices
- Blood Indices
Whilst there are numerous methods for assessing the hydration status of athletes, each of them have varying levels of validity, reliability and practicality.
Why is hydration testing important?
It is important to maintain the body’s state of homeostasis as much as possible before, during and after exercise, as this helps to ensure the athlete can perform at their very best and recover adequately.
In terms of fluid balance, the goal prior to exercise is to have the body in its euhydrated state (7). Pre-performance (e.g. training or competition) hydration testing can, therefore, determine if the athlete is in a sufficient state of hydration, and thus ready to participate at their absolute optimum.
Dehydration and Performance
During exercise, a 2% or higher reduction in an athlete’s body weight has been shown to decrease both aerobic and cognitive performance (8, 9).
There is evidence to suggest that an increase in an athlete’s core temperature can decrease their motor-neural output during exercise. This can have a negative effect on their exercise tolerance time and their drive to exercise in the heat due to serotonergic mechanisms (10).
As mentioned before, dehydration can affect aerobic performance. This is because body water deficits can result in an increase in cardiovascular strain due to an increased heart rate and decreased stroke volume; ultimately resulting in a decrease in cardiac output. Dehydration can also lower cardiac filling due to a reduction in blood volume, this is often accompanied by a rise in skin blood flow and skin compliance (8).
There have been mixed results when reporting the relationship between dehydration and muscular strength and power. Whilst there have been reports that dehydration does affect muscular function (11, 12), there are also contradicting results (13, 14). This suggests that this is an area for future research in order to determine if there is a relationship between dehydration and muscle functioning.
Dehydration and Injury
The previous section explained how dehydration can affect the central nervous system, effectively causing fatigue. However, there are other health risks that dehydration poses to an athlete, such as cramps, hyponatraemia and heat stroke (this will be covered in the next section).
Despite the extremely high prevalence of exercise-associated muscle cramps (EAMC), the aetiology of this condition is not well understood (15). There are three hypotheses to determine the aetiology of EAMC:
- Dehydration hypothesis
- Electrolyte depletion hypothesis
- Altered neuromuscular hypothesis
Whilst there is not an overwhelming amount of scientific evidence for either of the three (15), it seems as though the altered neuromuscular hypothesis has the more likely pathophysiological mechanism for EAMC. Basically, exercise will cause muscle fatigue which will, in turn, increase excitatory afferent activity and decrease inhibitory afferent activity. This leads to altered neuromuscular control which then affects alpha motor neuron activity leading to EAMC. Although, it is important to recognise the number of factors that will determine the severity (e.g. exercise intensity, duration, conditioning level) (15).
Prolonged exercise (> 5 hrs) can cause hyponatraemia, which is defined as having a diluted blood sodium concentration in the body (7). Hyponatraemia is caused when an individual consumes fluids low in sodium or sodium-free water and does not replace the necessary electrolytes lost (16). As a result, marathon runners seem to be prone to hyponatraemia when they do not implement effective hydration strategies (17).
There also seems to be a relationship between the severity of the symptoms (e.g. nausea, headache, confusion and fatigue) and the amount by which blood sodium concentration have fallen (18).
Dehydration and Death
As previously touched upon, there can be serious health risks for individuals who exercise whilst dehydrated. In some extreme cases, there have even been several reports of death due to heat stroke, with dehydration said to be a contributing factor (19).
Heat stroke is diagnosed when the following criteria are met (16):
- Body temperature reaches 40.5 °C or greater
- Presence of cognitive function impairment
- Anidrosis (absence of sweating)
To prevent this from occurring, there are natural neurophysiological processes in place to maintain homeostasis. Thermoregulation is the process in which heat is dissipated from the body in order to maintain an optimal core temperature (37 °C) (20). A rise of just 1° can activate the body’s thermoregulatory centre, which can then act to reduce the body temperature through several mechanisms (20), one of which being perspiration (i.e. sweating).
It is proposed that dehydration reduces cardiovascular function, which, therefore leads to a decrease in skin blood flow and the inability to lose heat via sweat (8, 21, 22).
To summarise, given the impact hydration can have not only on performance but also on health, this firmly demonstrates the importance of having some form of hydration strategy in place to ensure athletes are well-informed and monitored.
How is hydration measured?
There are a number of different ways to measure an athlete’s hydration status, each with its own levels of validity, reliability and practicality.
Urine Specific Gravity (USG)
Urine Specific Gravity (USG) is the density of a urine sample compared to the density of water (6). The density of the sample is determined by its osmolality, as well as the concentration of a number of molecules such as urea, protein and glucose. There are three main methods of testing an individual’s USG (6).
- Hydrometry: The density of the sample can be tested using a weighted glass float (6). This method is considered to be inaccurate and impractical due to daily calibration being needed, a large urine sample, and also because it is temperature sensitive (6, 23).
- Refractometry: This involves a light being passed through the sample and measuring how much the beam has refracted (23). In contrast to hydrometry, it requires a smaller sample and internally corrects for the temperature; making it a more practical and inexpensive option for measuring hydration.
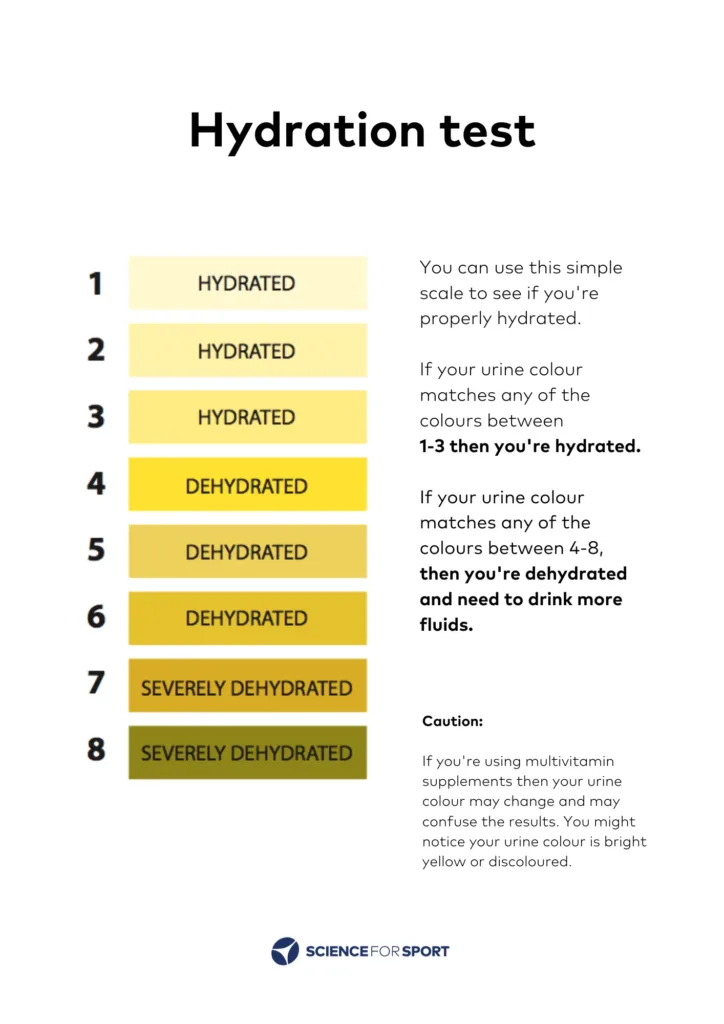
- Reagent Strips: These strips offer a more simple approach than refractometry and hydrometry. The strips react to the number of hydrogen ions released in the sample, which ultimately affects the pH and is detected by the Bromthymol blue contained in the strip (23). As the pH decreases (indicating an increase in H+ ions), the strip changes colour to a more yellow-green. A colour kit can then be used to estimate the sample’s USG.
Bioelectrical Impedance Analysis (BIA)
Bioelectrical Impedance Analysis testing can take the form of many types, these include:
- Single Frequency BIA
- Multi-Frequency BIA
- Bioelectrical spectroscopy (BIS)
- Segmental BIA
- Localized BIA
- Bioelectrical impedance vector analysis (BIVA).
This article will mainly focus on SF-BIA because it is of relatively low cost, portability and practicality (24). Whilst it has been criticised for its poor accuracy in subjects that have significantly altered hydration levels (e.g. in clinical settings), it can still be used to estimate total body water (TBW) in subjects that are normally hydrated; such as athletes (24).
The science behind this approach is quite simple: it involves an alternating current passing through the body (50 kHz) and the resistance to the current is measured (6). There are a number of ways that this can done, such as using gel electrodes that are placed on both wrists and ankles or using a stand-on platform with hand-held devices (6). The data received depends on the model of equipment used, some devices provide an estimation of total body water stores, whereas others provide raw data and calculations must be used to further predict the athlete’s body composition (6).
This method is seen to be safe, rapid and easy to administer, however, the machine used to calculate the estimations can be quite costly. The positive side of that is that there is minimal technical skill required to work the machine. The accuracy and precision of results can be affected by a number of factors (25) such as:
- Food, drink and alcohol: fasting for > 8 hr is recommended
- Generator: correct calibration
- Electrode position: clean with alcohol first, with minimum of 5 cm between electrodes
- Physical exercise: no exercise for > 8 hr prior
- Subjects: height and weight need to be correctly calibrated using a stadiometer and scales closest to the nearest 0.5 cm and 0.1 kg respectively.

Body Weight Changes
Body weight changes have been used in the past to measure acute changes in hydration status (26). This method’s popularity with sporting clubs can be accredited to the fact that it is a simple, non-expensive and non-invasive tool that can provide a quick estimate of an athlete’s so-called hydration status.
The principle behind measuring an athlete’s body weight before and after exercise to estimate hydration status is relatively simple. It is assumed that 1 ml of sweat represents 1 g of mass lost (2). The mass loss can then be used to express the post-training BW as a percentage of pre-training BW through the following equation:
Mass Loss (%) = [BW (post) / BW (pre)] x 100
For example, if an athlete weighed in at 78 kg before training and weighed out at 76.8 kg after training, the equation would read [76.8 kg / 78 kg] x 100 = 98.5 %, meaning a mass loss of 1.5 %.
However, it is important to note that there are many factors that could limit the reliability and validity of the results. Using this method assumes that all mass lost during exercise is only due to sweat, but many other factors can contribute towards mass loss (26). Some of these include:
- Respiration
- Substrate oxidation
- Urination and excrement
From a practical perspective, this method uses minimal equipment, is quick to conduct, is cost-effective, and can provide a quick estimation of an athlete’s hydration status immediately after exercise. However, it is important to understand the different variables that can affect the reliability of the results.
Urinary Indices
Hydration status can be measured by monitoring characteristics such as volume, colour conductance and osmolality (6). Under normal conditions, the amount of urinary volume excreted can range from 1.5-2.5 L/day, with the colour a pale to light yellow and an osmolality of < 500 mOsm/L (27). When exercise commences, water conservation mechanisms are activated in the kidneys to ensure that both plasma volume and intracellular water are maintained, this has an effect on the aforementioned urinary characteristics.
Measuring the athlete’s urinary volume quantitatively (i.e. how much the athlete has urinated that day) requires a large amount of compliance and cooperation from the athlete; however, a more qualitative method can be used, such as asking the athlete the frequency of urination during the day (6). Both approaches require a degree of athlete education to ensure that the data collected is accurate.
Measuring urine osmolality involves the collection of urine and using a freezing point osmometer to determine the number of solutes (e.g. NaCl) per kg of solution (6). This requires a trained technician and also expensive equipment, though there is an alternative. The use of a Sparta 5 Conductance Metre has been validated in previous research (28). This method uses a 5-point scale to provide feedback regarding the conductance of a person’s urine and provides immediate feedback which is simple to use.
A 6-point Likert Scale can be used to estimate hydration status through urinary colour (29). Copies of the scale can be distributed between athletes. This is non-invasive, non-expensive and simple to use, however, the athlete must be educated to ensure that they use to scale correctly and must take note of the results.
These methods to estimate hydration status through urinary indices may prove invalid if there are large acute ingestions of fluid after exercise (30, 31). This may produce diluted urine and mask their true hydration status (6). Methods must be put in place to ensure that hydration testing is completed as soon as possible after exercise so that the data collected is as accurate and precise as possible.
Blood Indices
It is thought that a number of blood-borne indices can be used to test the dehydration status of an athlete. Hypertonic dehydration (e.g. from profuse sweating) can be detected through changes in plasma osmolality and plasma sodium (30, 32), whilst hypotonic or isotonic dehydration can be detected through serial haematocrit or haemoglobin measurements (33).
This method requires a properly trained professional to ensure that safe and sterile measurements are taken with the appropriate laboratory equipment. Examples of which are outlined below:
- Freezing point osmometer (Plasma osmolality)
- Ion selective electrode (Plasma sodium)
- Centrifuge and capillary tubes (Haematocrit)
- Spectrometer (Haemoglobin)
This method of hydration testing can be costly, invasive and labour-intensive (6). Due to the fact that it requires blood sampling, there will always be a risk of infection, bruising and vein damage.
There have been studies that clearly show that a loss of > 3 % BW during exercise results in an increase in plasma osmolality (30, 32). However, there is contradicting research regarding the sensitivity of blood osmolality when < 3 % BW has been lost (34). From this study, they concluded that urinary measures may be more accurate during conditions of mild dehydration; which other research supports (29). This could be due to the fact that urine is more concentrated to maintain normal blood chemistry during exercise (6). Adding further contradiction and complexity, one study even demonstrated that plasma osmolality was highly responsive to a reduction in BW by < 1 % (30).
Plasma sodium has been found to increase under conditions of dehydration (32). This study aimed to investigate the use of plasma sodium as a marker of dehydration during exercise in heat. It involved 2 hours of cycling (3.7 % BW lost) and a further 21 additional hours of fluid retention. Results show an increase in plasma sodium from baseline measurements, and an extra 20 minutes of cycling (1.5 % BW lost) showed a further increase in plasma sodium.
One study compared haematocrit and haemoglobin levels to levels of total body water both before and after an exercise intervention lasting 14 days (33). It showed that blood indices correlated with total body water throughout the study, suggesting that these may be useful for situations of hypotonic and isotonic dehydration.
Whilst plasma osmolality, blood sodium, haematocrit and haemoglobin may provide accurate information regarding hydration status, the limitations outlined earlier seem to outweigh the benefits at this point in time. Further research and engineering are needed to provide a more practical approach when using these measurements.
Are there any issues with hydration testing?
Limitations regarding hydration testing primarily appear to be related to its practicality in the field. For example, it would be impractical to have an entire AFL or Rugby League team use BIA after every training session or to use USG to estimate hydration level. Unfortunately, due to the current technology, to implement a method that is appropriate/practical (e.g. BW changes), measurement accuracy will, most likely, be sacrificed. Coaches, fitness and medical staff must communicate what they feel is the most appropriate method for their particular sport.
A further issue with hydration testing can be the priority that this measurement takes in the eyes of the fitness and medical staff. Coaches outside of an elite environment may not have the time or resources to hydration test their athletes, potentially putting their performance and health at risk.
Is future research needed with hydration testing?
Future research in the area of hydration testing should focus on determining if current methods can be altered so that they can provide an even more valid and reliable measurement as well as addressing the following issues:
- The effects of acute rehydration after exercise as net weight gain is not an acceptable method of rehydration assessment as it fails to monitor fluid replacement in both the extracellular and intracellular compartments of the body (6). This is where measures of urinary and blood parameters can play a part in determining an individual’s hydration status both before and after exercise.
- Indices such as potassium, sodium and protein may be appropriate hydration tests (6), but no methods are currently available which are simple, quick and low-cost.
Conclusion
Hydration testing is a very important part of any athletic programme and can prevent serious performance and health deficiencies. There are methods available which are valid, inexpensive and non-time-consuming, but the confounding variables that may affect results must be addressed. The method that best suits the practitioner/coach and their environment will depend on several factors; such as the resources available and the time-cost.
Future research is required to assess whether urinary and blood indices can be used as hydration tests in a practical sense.
- Sawka, MN and Young, AJ. Physiological Systems and Their Responses to Conditions of Heat and Cold. In: ACSM’s Advanced Exercise Physiology. 535-563, 2005. http://www.dtic.mil/docs/citations/ADA448266
- Sawka, MN. Burke, LM. Eichner, ER. Maughan, RJ. Montain, SL and Stachfield, NS. American College of Sports Medicine position stand: Exercise and Fluid Replacement. Medicine and Science in Sports and Exercise (39): 377-90, 2007. https://www.ncbi.nlm.nih.gov/pubmed/17277604
- Casa, DJ. Clarkson, PM and Roberts, WO. American College of Sports Medicine roundtable on hydration and physical activity: consensus statements. Current Sports Medicine Reports (4): 115-127, 2005. https://www.ncbi.nlm.nih.gov/pubmed/15907263
- Institute of Medicine. Washington D.C. Dietary Reference Intakes for Water, Sodium, Chloride, Potassium and Sulfate. National Academy Press. [Book]: 73-185, 2005.
- Sawka MN and Pandolf KB. Effects of body water loss on physiological function and exercise performance. Perspectives in Exercise Science and Sports Medicine (3):1-38, 1990.
- Opplinger, RA and Bartok, C. Hydration Testing of Athletes. Sports Medicine (32): 959-71, 2002. https://www.ncbi.nlm.nih.gov/pubmed/12457417
- Powers, SK and Howley, ET. Exercise Physiology [Textbook], 2014.
- Cheuvront, SN. Carter III, R and Sawka, MN. Fluid balance and endurance exercise performance. Current Sports Medicine Reports (3): 202-8, 2003. https://www.ncbi.nlm.nih.gov/pubmed/12834575
- Cian, C. Koulmann, N. Barraud, PS. Raphel, C. Jimenez, C and Merlin, B. Influence of variations in body hydration on cognitive function: effect of hyperhydration, heat stress, and exercise-induced dehydration. Journal of Psychophysiology (14):29–36, 2000. https://www.researchgate.net/publication/232561018_Influence_of_variations_in_body_hydration_on_cognitive_function_Effect_of_hyperhydration_heat_stress_and_exercise-induced_dehydration
- Cheuvront, SN and Sawka, MN. Physical Exercise and Exhaustion from Heat Strain. Journal of the Korean Society of Living Environment System (8): 134-145, 2001. http://www.dbpia.co.kr/Journal/ArticleDetail/NODE00934348
- Schoffstall, JE. Branch, JD. Leutholtz, BC and Swain, DE. Effects of dehydration and rehydration on the one-repetition maxmimum bench press of weight trained males. Journal of Strength and Conditioning Research (15):102-108, 2001. https://www.ncbi.nlm.nih.gov/pubmed/11708691
- Viitasalo, JT. Kyrolainen, H. Bosco, C and Alen, M. Effects of rapid weight reduction on force reproduction and vertical jumping height. International Journal of Sports Medicine (8):281-285, 1987. https://www.ncbi.nlm.nih.gov/pubmed/3667026
- Judelson, DA. Maresh, CM. Farrell, MJ. Yamamoto, LM. Armstrong, LE. Kraemer, WJ. Volek, JS. Speirring, BA. Casa, DJ and Anderson, JM. Effect of hydration state on strength, power and resistance exercise performance. Medicine and Science in Sports and Exercise (39): 1817-1824, 2007. https://www.ncbi.nlm.nih.gov/pubmed/17909410
- Evetovich, TK. Boyd, JC. Drake, SM. Eschbach, LM. Magal, M. Soukup, JT. Webster, MJ. Whitehead, MT and Weir, JP. Effect of Moderate Dehydration on torque, electromyography and mechanomyography. Muscle Nerve (26): 225-231, 2002. https://www.ncbi.nlm.nih.gov/pubmed/12210387
- Schwellnus, MP. Cause of Exercise Associated Muscle Cramps (EAMC) – altered neuromuscular control, dehydration or electrolyte depletion. British Journal of Sports Medicine (43): 401-408, 2008. https://www.ncbi.nlm.nih.gov/pubmed/18981039
- Taylor, NAS and Groeller, H. Physiological bases of Human Performance during Work and Exercise [Textbook]. 2008.
- Davis, DP. Videen, JS. Marino, A. Vike, GM. Dunford, JV. Van Camp, SP. Maharam, LG. Exercise associated hyponatremia in marathon runners: a two-year experience. The journal of Emergency Medicine (21): 47-57, 2001. https://www.ncbi.nlm.nih.gov/pubmed/11399389
- Knochel, JP. Clinical Complications of body fluid and electrolyte balance. Body fluid balance: Exercise and Sport [Textbook], 1997.
- Mueller FO. Annual survey of football injury research: 1931- 2001. Chapel Hill (NC): National Center for Catastrophic Sports Injuries, 2002.
- Bouchama, A and Knochel, JP. Heat Stroke. The New England Journal of Medicine (346): 1978-1988, 2002. http://www.nejm.org/doi/full/10.1056/NEJMra011089
- Sawka, MN. Young, AJ. Francesconi, RP. Muza, SR and Pandolf, KB. Thermoregulatory and blood responses during exercise at graded hypohydration levels. Journal of Applied Physiology (59): 1394-1401, 1985. https://www.ncbi.nlm.nih.gov/pubmed/4066570
- Stover, EA. Zachweija, J. Stofan, J. Murray, R and Horswill, CA. Consistently high urine specific gravity in adolescent American football players and the impact of an acute drinking strategy. International Journal of Sports Medicine (27): 330-335, 2006. https://www.ncbi.nlm.nih.gov/pubmed/16572377
- Brunzel, NA. Fundamentals of Urine and Body Fluid Analysis [Textbook], 1994.
- Mialich, MS. Sicchieri, JMF and Junior, AFJ. Analysis of Body Composition: A Critical Review of the Use of Bioelectrical Impedance Analysis. International Journal of Clinical Nutrition (2): 1-10, 2014. http://pubs.sciepub.com/ijcn/2/1/1/
- Kyle, UG. Bosaeus, I. De Lorenzo, AD. Deurenberg, P. Elia, M. Gomez, JM. Heitmann, BL. Kent-Smith, L. Melchiar, JC. Pirlich, M. Scharfettor, H. Schols, AMWJ and Pichard, C. Bioelectrical Impedance Analysis-part II: Utilization in Clinical Practice. Clinical Nutrition (23): 1430-53, 2004. https://www.ncbi.nlm.nih.gov/pubmed/15556267
- Maughan, RJ. Shirreffs, SM and Leiper, JB. Errors in the Estimation of Hydraion Status from Changes in Body Mass. Journal of Sport Sciences (25): 797-804, 2007. https://www.ncbi.nlm.nih.gov/pubmed/17454547
- Strasinger, SK. Urinalysis and Body Fluids [Textbook], 1994.
- Shireffs, SM and Maughan, RF. Urine Osmolality and conductivity as indices of hydration status in athletes in the heat. Medicine and Science in Sport and Exercise (30): 1598-1602, 1998. https://www.ncbi.nlm.nih.gov/pubmed/9813872
- Armstrong, LE. Maresh, CM. Casellani, JW. Bergeron, MF. Kenefick, RW. LaGasse, KE. Riebe, D. Urinary indices of hydration status. International Journal of Sports Nutrition (4): 265-279, 1994. https://www.ncbi.nlm.nih.gov/pubmed/7987361
- Popowski, CA. Opplinger, RA. Lambert, P. Johnson, RF. Johnson, KA. Gisolf, CV. Blood and urinary measures of hydration status during progressive acute dehydration. Medicine and Science in Sports and Exercise (33): 747-753, 2001. https://www.ncbi.nlm.nih.gov/pubmed/11323543
- Kovacs, EMR. Seden, JMG and Browns, F. Urine colour, osmolality and specific electrical conductance are not accurate measures of hydration status during post exercise rehydration. Journal of Sports Medicine and Physicial Fitness (39): 47-53, 1994. https://www.ncbi.nlm.nih.gov/pubmed/10230169
- Armstrong, LE. Soto, JA. Hacker, FT Jr. Casa, DJ. Kavouras, SA. Maresh, CM. Urinary Indices during dehydration, exercise and rehydration. International Journal of Sport Nutrition (8): 345-355, 1998. https://www.ncbi.nlm.nih.gov/pubmed/9841955
- Hackney, AC. Coyne, JT. Pozos, R. Feith, S. Seale, J. Validity of urine-blood hydrational measures to assess total body water changes during mountaineering in the sub-arctic. Artic Medical Research (54): 69-77, 1995. https://www.ncbi.nlm.nih.gov/pubmed/7639888
- Francescone, RP. Hubbard, RW. Szlyk, PC. Schnakenberg, D. Carlson, D. Leva, N. Sils, I. Hubbard, L. Please, V. Young, J. Urinary and hemotalogic indexes of hypohydration. Journal of Applied Physiology (62): 1271-1276, 1987. https://www.ncbi.nlm.nih.gov/pubmed/3571082