Contents of Article
- Summary
- What is a DEXA scan?
- How does DEXA scanning determine body composition?
- Are DEXA scans valid and reliable?
- Are there issues with DEXA scans?
- Is future research needed with DEXA scans?
- Conclusion
- References
- About the Author
Summary
Dual-energy X-ray Absorptiometry (DEXA) scans determine body composition by passing low-radiation X-ray beams through tissues, with varying energy absorption allowing the practitioner to determine both tissue type and quantity. DEXA scans are the gold standard method for measuring bone density and are used for diagnosing bone conditions in clinical and sports settings.
Despite the potential for individual error, DEXA scans appear to be a valid measure when comparing mean results against the criterion four-compartment method (fat mass, total body water, bone mineral mass, residual mass). The reliability of DEXA scans can vary, however, the error can be minimised by standardising the measurement conditions and equipment, in addition to following best practice.
Current research suggests that DEXA scanning can be a valuable assessment tool for practitioners intending to measure body composition (e.g. levels of body fat).

What is a DEXA scan?
Dual-energy X-ray absorptiometry (DEXA) is a measurement technique used to determine bone mineral density. DEXA is increasingly being used to determine body composition in a variety of settings, including obesity [1], sarcopenia [2], and elite sport [3].
A DEXA scan involves the passing of low-radiation X-ray beams through bones, and the amount of energy that is absorbed allows for the determination of the density of the bone. Radiation energy per pixel is established and converted to g/cm for a given area. The number of pixels in each area is determined, and the amount of bone in each pixel is calculated, allowing for the calculation of bone density in specific bones [4].
Two energies are used to estimate soft tissue absorption, separate from the bone. The DEXA scan creates a two-dimensional image, preventing the measure of bone depth.
How does DEXA scanning determine body composition?
There are several methods used to determine body composition, and each method has pros and cons regarding the accuracy, financial cost, practicality, and other factors. DEXA scans provide a 3-compartmental model for body composition estimation. The three compartments are;
- Bone mineral
- Fat
- Other fat-free mass that isn’t bone
A criticism of 2-compartment models (dividing weight into fat mass and fat-free mass) is that errors occur due to assumptions of the density in fat mass and fat-free mass (e.g. variations in bone density have been identified between different ethnicities [5]). This, therefore, demonstrates a potential advantage of DEXA scan use.
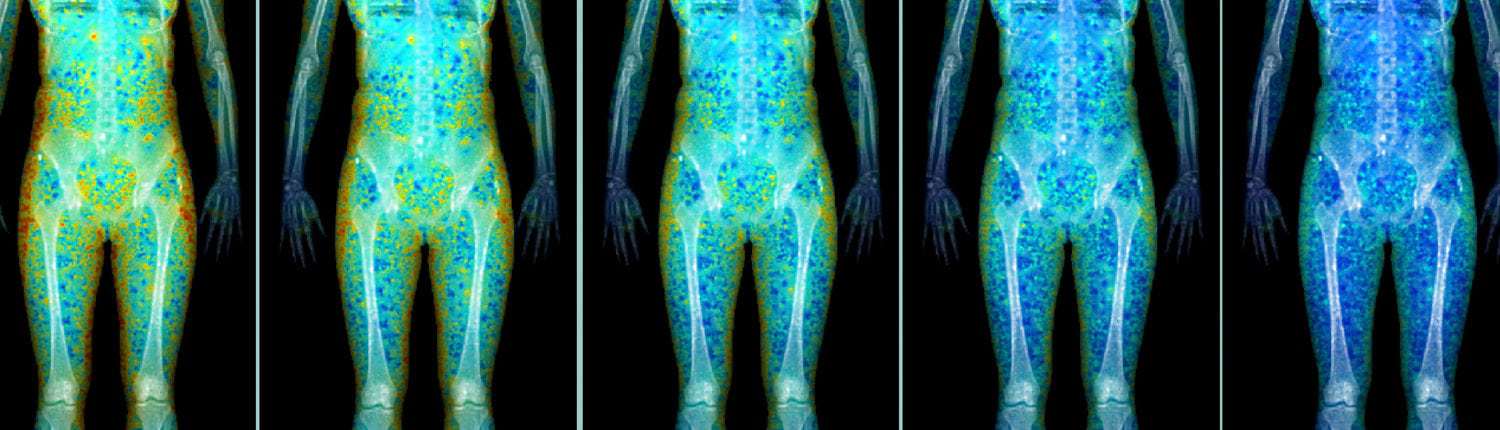
DEXA scanning offers a number of potential benefits for body composition assessment. The scan itself involves the movement of a ‘machine arm’ across the length of the body being measured. A full body scan takes approximately eight minutes, making it a time-efficient, non-invasive measure of body composition. The scanner can also be adjusted to measure a single body part or segment, providing regional estimations of body composition.
DEXA scans are used to determine bone mineral density. DEXA scanning is considered the gold standard method for determining bone mineral density and is thus used in the assessment of osteopenia (lower than average bone density) and osteoporosis (much lower bone density, risk of bone fracture). This can be important in certain athletic populations with a greater risk of low bone density and osteoporosis, such as long-distance runners (predominantly females).
Therefore, the use of serial DEXA body composition measurement may provide data regarding athlete conditioning, training outcomes, and rehabilitation progress, as well as indicate increases in fat mass, or decreases in skeletal muscle mass or bone mineral density that could be detrimental to athletic performance [6].
Are DEXA scans valid and reliable?
The validity (the agreement between the true value and a measurement value) of body composition is key to determining the precision of a measurement. A multi-compartment model, specifically the four-compartment model (fat mass, total body water, bone mineral mass, residual mass), is regarded as the criterion method in determining body composition, and thus this model is often used in comparison when assessing the validity of DEXA measurements [7]. Despite this, there is a relative lack of validation studies using these comparisons, predominantly due to the time, labour, and financial cost involved [7].
The validity of DEXA scans when compared to the four-compartment model is currently equivocal. A study by Arngrimsson et al. (2000) in male and female distance runners reported that DEXA underestimated body fat measurements by around 2 % [8]. This finding was replicated in a study by Van der Ploeg et al., (2003) in a healthy adult population [9], and slightly less than the 4 % difference in trained men found by Withers et al. (1998) [10]. Fat-free mass was also reported to be overestimated by approximately 2.5 kg [10].
Conversely, other research has shown an overestimation of body fat by 3-4 %, and an underestimation of fat-free mass by up to 3 kg [3, 11]. The differences in the reported validity of DEXA scans for body composition may partly be due to differences in software, manufacturer, and the wide range of body composition values across various cohorts. It is worth noting that although current research is conflicting, it is commonly assumed that DEXA is a valid technique for the assessment of body composition.
It is also important to consider the validity of DEXA results not only for cross-sectional data (observational data at one given time point) but also when assessing changes in body composition over time, as this is often of interest to the sports science practitioner. Early research in this area used the novel method of scanning participants, before placing lard samples on the participants to simulate a gain in adipose tissue. One study showed that fat mass and lean body mass measurements were not significantly different from the expected change following the placement of 8.8 kg of lard on healthy female subjects [11]. Another study also reported measurements in line with expectations when 11.1kg was added, however, there was evidence that fat mass was underestimated by 1.9 % when the amount of lard added was increased to 22.2 kg [12].
Data on DEXA use to assess body composition in athletic populations is scarce. Van Marken et al., [13] showed no difference in mean body composition change between the four-compartment model and DEXA scans in male bodybuilders. This finding was replicated by Santos et al., [3] in male judo competitors. Despite these findings, both studies reported that individual error rates of 4% for body fat measurement, highlighting the large individual differences within measurements.
The reliability (the reproducibility of the observed value when the measurement is repeated) of DEXA scanning is important for determining the precision of a single measurement, as well as the ability to detect change over multiple measurements. Despite the various benefits of DEXA scanning for body composition assessment, it is not without error. Inconsistent results can occur when using scanners from different manufacturers [14], as well as two scanners produced by the same manufacturer [15]. Software updates may also alter body composition results due to algorithm variation [16]. Differences in the x-ray beam used can also contribute to error; pencil beams and fan beam DEXA systems have been shown to provide significantly different body composition test results, limiting comparison between the two [17].
Biological variation may also affect reliability in DEXA measurements, particularly in athletic populations. The effects of fluid intake on body composition have been studied previously, showing that fluid intake of 0.8-2.4 L of water can significantly increase lean mass estimates in the trunk region [18]. Similar results were reported by Thomsen et al. (1998) [19], showing that estimates of lean body mass were increased by over 1 kg per hour following a standard meal weighing 1311 g, as well as after drinking 1 L of water.
Changes in any of these variables are not uncommon in athletic populations and may mask or give the false impression of changes in skeletal muscle mass. Bone et al. (2016) [20] reported that glycogen and creatine loading increased lean mass values by 2.1 % and 1.3 %, respectively. A variation in hydration status of 5 % has also been shown to alter DEXA predictions of body fat by 3 % [21]. As manipulation of these variables is commonplace with athletes, standardisation is key to accurately detect meaningful change.
Are there issues with DEXA scans?
Practically, DEXA scanning may also have some issues. The cost and accessibility of DEXA scanning can be an issue, particularly for sports teams that have large squad numbers and limited budgets. Furthermore, DEXA scans do use ionizing radiation, and although the absolute dose per scan is minimal, it may be advisable to minimise the number of scans performed per year on one individual; limiting the quantity of body composition data that can be acquired [22]. In these instances, it may be prudent to use more basic, cost-effective methods of body composition assessment such as skinfold calipers.
A further issue (particularly with some athletic populations) can be the size of DEXA scanners, as they may not be able to accommodate individuals who are taller or broader than the scanning area. For tall athletes, one technique is allowing the athlete to bend their knees, thus allowing the head and feet to be included in the scan. However, this has been shown to lead to significant error, with fat mass (9.2 %) and lean body mass (4 %) both vastly overstated when compared to a standard measure [23]. Other methods involve the summation of separate scans to achieve a total body measurement, however, this method also leads to substantial error [24].
As mentioned previously, reliability may be an issue if best practice is not observed, and measurements are not correctly standardised [25]. Measurements of fat and fat-free tissue are also made on the assumption that fat-free mass hydration is constant at 73 % [26], however, the hydration of fat-free mass has been suggested to be 72-74.5 % [27]. Although not necessarily an issue, as all measurement methods have an inherent error due to assumptions, these variations may potentially cause detectable variability in the estimation of fat-free mass.
The Best Practice Protocol for the assessment of whole body composition by DEXA
A standardised protocol for the use of DEXA to measure body composition of athletes is necessary, but there is an absence of a universal approach to this need. Nana et al. (2014) published a best practice protocol of DEXA body composition assessment suitable for use in a real-life athlete setting – with known reliability which has been optimised in terms of the balance between the effort required to achieve it and the benefits of its precision [30]. This protocol, presented below, was developed from first principles, in conjunction with pilot work and a series of studies of sources of measurement variability.
Although this protocol ensures maximum precision, it poses some practical costs and the burden on both the athletes and the technician that need to be balanced against the potential value of the additional precision gained. As an example, if a player turns up late and the technicians rush through the calibration of the scan, or the athlete is not aligned in the scanning area correctly, it can skew the results.
Is future research needed with DEXA scans?
In terms of body composition assessment, a greater dataset of reference body composition data for athletes in various sports (and various positions/roles within these sports) is needed. To this end, the ability of DEXA scans to also provide segmental analysis may provide practitioners to identify ‘regions of interest’ that may determine successful performance in these sports or roles. This also may allow greater insight into the effects of an intervention that has been utilised. For example, if lower-body musculature is identified as important, the ability to track changes in skeletal muscle at this site could be useful.
Furthermore, the Best Practice Protocol should be considered a recommended standard until future work allows further refinements to be made. Furthermore, studies which involve DEXA measurements of body composition should report details of how their scanning techniques conform to this or other standardisation procedures.
Conclusion
Despite the inherent limitations of body composition assessment via DEXA scan, with considered application and interpretation in the right context it can provide a robust and suitably reliable assessment of body composition, particularly in comparison to other body composition assessment methods.
The ability of DEXA scans to provide greater levels of detail regarding bone density and segmentation measurements makes it an attractive choice to practitioners who have the logistic and financial means.
- C. Zalesin, B. A. Franklin and M. A. Lillystone. (2010). ‘Differential loss of fat and lean mass in the morbidly obese after bariatric surgery’. Metabolic Syndrome Related Disorders, 8(1): pp. 15-20. https://www.ncbi.nlm.nih.gov/pubmed/19929598
- J. Cruz-Jentoft, J. P. Baeyens and J. M. Bauer. (2010). ‘Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on sarcopenia in older people’. Age Ageing, 39(4): pp. 412-423. https://www.ncbi.nlm.nih.gov/pubmed/20392703
- A. Santos, A. M. Silva and C. N. Matias(2010). ‘Accuracy of DEXA in estimating body composition in elite athletes using a four compartment model as the reference method’. Nutrition and Metabolism, 7: pp. 22-31. https://www.ncbi.nlm.nih.gov/pubmed/20307312
- Berger A. (2002). ‘Bone mineral density scans’. BMJ (Clinical research ed.), 325(7362): 484. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1124002/
- B. Araujo, T. G. Travison, S. S. Harris, M. F. Holick, A. K. Turner and J. B. McKinlay. (2007). ‘Race/ethnic differences in bone mineral density in m’. Osteoporosis International, 18: pp. 943-953. https://www.ncbi.nlm.nih.gov/pubmed/17340219
- Buehring, D. Krueger, J. Libber, B. Heiderscheit, J. Sanflippo, B. Johnson, I. Haller and N. Binkley. (2014). ‘Dual-Energy X-Ray Absorptiometry measured regional body composition least significant change: Effect of region of interest and gender in athletes’. Journal of Clinical Densitometry: Assessment and Management of Musculoskeletal Health, 17: pp. 121-128. https://www.ncbi.nlm.nih.gov/pubmed/23643968
- R. Ackland, T. G. Lohman, J. Sundgot-Borgen, R. J. Maughan, N. L. Meyer, A. D. Stewart and W. Muller. (2012). ‘Current status of body composition assessment in sport: review and position statement on behalf of the ad hoc research working group on body composition health and performance, under the auspices of the I.O.C. Medical Commission’. Sports Medicine, 42(3): pp. 227-249. https://www.ncbi.nlm.nih.gov/pubmed/22303996
- Arngrimsson, E. M. Evans, M. J. Saunders, C. L. Ogburn, R. D. Lewis and K. J. Cureton. (2000). ‘Validation of body composition estimates in male and female distance’. American Journal of Human Biology, 12: pp. 301-314. https://www.ncbi.nlm.nih.gov/pubmed/11534021
- E. Van der Ploeg, R. T. Withers and J. Laforgia. (2003). ‘Percent body fat via DEXA: comparison with a four-compartment model’. Journal of Applied Physiology, 94(2), pp. 499-506. https://www.ncbi.nlm.nih.gov/pubmed/12531910
- T. Withers, J. LaForgia, R. K. Pillans, N. J. Shipp, B. E. Chatterton, C. G. Schultz and F. Leaney. (1998). ‘Comparisons of two-, three-, and four-compartment models of body composition analysis in men and women’. Journal of Applied Physiology, 85: pp. 238-245. https://www.ncbi.nlm.nih.gov/pubmed/9655781
- L. Svendsen, J. Haarbo, C. Hassager and C. Christiansen. (1993). ‘Accuracy of measurements of body composition by dual-energy x-ray absorptiometry in vivo’. American Journal of Clinical Nutrition, 57: pp. 605-608. https://www.ncbi.nlm.nih.gov/pubmed/18936958
- R. Madsen, J. E. Jensen and O. H. Sorensen. (1997). ‘Validation of a dual-energy x-ray absorptiometer: measurement of bone mass and soft tissue composition’. European Journal of Applied Physiology, 75: pp. 554-558. https://www.ncbi.nlm.nih.gov/pubmed/8480673
- W. D. van Marken , F. Hartgens, N. B. Vollaard, S. Ebbing and H. Kuipers. (2004). ‘Body composition changes in bodybuilders: a method comparison’. Medicine and Science in Sport and Exercise, 36(3): pp. 490-497. https://www.ncbi.nlm.nih.gov/pubmed/15076792
- E. Pritchard , C. A. Nowson, B. J. Strauss, J. S. Carlson, B. Kaymacki and J. D. Wark (1993). ‘Evaluation of dual energy X-ray absorptiometry as a method of measurement of body fat’. European Journal of Clinical Nutrition, 47: pp. 216-228. https://www.ncbi.nlm.nih.gov/pubmed/8458318
- Lantz, G. Samuelson, L. E. Bratteby, H. Mallmin and L. Sjostrom. (1999). ‘Differences in whole body measurements by DXA-scanning using two Lunar DPX-L machines’. International Journal of Obesity Related Metabolic Disorders, 23(7): pp. 764-770. https://www.ncbi.nlm.nih.gov/pubmed/10454112
- M. Lewiecki, N. Binkley and S. M. Petak. (2006). ‘DXA quality matters’. Journal of Clinical Densitometry, 9: pp. 388-392. https://www.ncbi.nlm.nih.gov/pubmed/17097522
- Henzell, S. S. Dhaliwal, R. I. Price, F. Gill, C. Ventouras, C. Green, F. Da Fonseca, M. Holzherr and R. Prince. (2003). ‘Comparison of pencil-beam and fan-beam DXA systems’. Journal of Clinical Densitometry, 6(3), pp. 205-210. https://www.ncbi.nlm.nih.gov/pubmed/14514988
- F. Horber, F. Thomi, J. P. Casez, J. Fonteille and P. Jaeger. (1992). ‘Impact of hydration status on body composition as measured by dual-energy x-ray absorptiometry in normal volunteers and patients on haemodialysis’. The British Journal of Radiology, 65: pp. 895-900. https://www.ncbi.nlm.nih.gov/pubmed/1422663
- K. Thomsen, V. J. Jensen and M. G. Henriksen. (1998). ‘In vivo measurement of human body composition by dual-energy x-ray absorptiometry’. European Journal of Surgery, 164: pp. 133-137. https://www.ncbi.nlm.nih.gov/pubmed/9537721
- L. Bone, M. L. Ross, K. A. Tomcik, W. G. Hopkins and L. M. Burke. (2016). ‘Manipulation of Muscle Creatine and Glycogen Changes DXA Estimates of Body Composition’. Medicine and Science in Sport and Exercise, 49(5): pp. 1029-1035. https://www.ncbi.nlm.nih.gov/pubmed/27898642
- M. Prior, K. J. Cureton, C. M. Modlesky, E. M. Evans, M. A. Sloniger, M. Saunders and R. D. Lewis. (1997). ‘In vivo validation of whole body composition estimates from dual-energy X-ray absorptiometry’. Journal of Applied Physiology, 83(2): pp. 623-630. https://www.ncbi.nlm.nih.gov/pubmed/9262461
- Damilakis, J. E. Adams, G. Gugliemi and T. M. Link. (2010). ‘Radiation exposure in X-ray-based imaging techniques used in osteoporosis,” European Radiology, 20(11): pp. 2707-2714. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2948153/
- M. Silva, F. Baptista and C. S. Minderico. (2004). ‘Calibration models to measure body composition in taller subjects using DXA’. International Journal of Body Composition Research, 2: pp. 165-173.
- Nana, G. J. Slater, W. G. Hopkins and L. M. Burke. (2012). ‘Techniques for undertaking DXA whole body scans to estimate body composition in tall and/or broad subjects’. International Journal of Sport Nutrition and Exercise Metabolism, 22: pp. 313-322. https://www.ncbi.nlm.nih.gov/pubmed/23011648
- Nana, G. J. Slater, A. D. Stewart and L. M. Burke. (2014). ‘Methodology Review: Using Dual-Energy X-ray Absorptiometry (DXA) for the assessment of body compositilon in athletes and active people’. International Journal of Sport Nutrition and Exercise, 25(2): pp. 198-215. https://www.ncbi.nlm.nih.gov/pubmed/25029265
- Pietrobelli, Z. Wang, C. Formica and S. B. Heymsfield. (1998). ‘Dual-energy x-ray absorptiometry: fat estimation errors due to variation in soft tissue hydration’. American Journal of Physiology, 274, pp. 808-816. https://www.ncbi.nlm.nih.gov/pubmed/25029265
- G. Lohman, M. Harris, P. J. Teixeira and L. Weiss (2000). ‘Assessing body composition and changes in body composition. Another look at dual-energy x-ray absorptiometry’. Annals of New York Academy of Sciences, 904, pp. 45-54. https://www.ncbi.nlm.nih.gov/pubmed/10865709
- E. Williams, J. C. Wells, C. M. Wilson, D. Haroun, A. Lucas and M. S. Fewtrell. (2006) ‘Evaluation of Lunar Prodigy dual-energy X-ray absorptiometry for assessing body composition in healthy persons and patients by comparison with the criterion 4- component model’. American Journal of Clinical Nutrition, 83: pp. 1047-1054. https://www.ncbi.nlm.nih.gov/pubmed/16685045
- R. Moon, J. M. Eckerson and S. E. Tobkin. (2009). ‘Estimating body fat in NCAA Division 1 female athletes- a five- compartment model validation of laboratory methods’. European Journal of Applied Physiology, 105: pp. 119-130. https://www.ncbi.nlm.nih.gov/pubmed/18936958
- Nana, A., Slater, G.J., Stewart, A.D., and Burke, L.M. (2015). Methodology review: using dual-energy X-ray absorptiometry (DXA) for the assessment of body composition in athletes and active people. Int J Sport Nutr Exerc Metab. 25(2):198-215. doi: 10.1123/ijsnem.2013-0228.